Abstract
Introduction: AIDS-related Diffuse large B-cell lymphoma (DLBCL) is a heterogeneous disease, with a variable response to chemotherapy depending on, and not limited to, cell of origin, double/triple hit, or MYC/BCL-2 co-expression status. Similar to DLBCL, AIDS-related DLBCL (ARL) with non-germinal center histology or MYC expression reports poorer response to treatment. In the immunocompetent population CD30+ DLBCL defines a histology with improved survival, however, the characteristics and outcomes of ARL expressing CD30 are not well studied.
Methods: We assessed 3 cohorts of ARL. The first cohort, consisted of of an immunohistochemistry tissue microarray (TMA) of 30 ARL patients, followed by two validation cohorts. The first validation was a TMA of 80 ARL, from the AIDS Cancer Specimen Resource. Both TMAs were stained for CD10, BCL6, MUM1, CD20, Ki67, EBER, MYC (by IHC) cut off at 40%, BCL2 (by IHC) cut off 50%, and CD30 (considered positive if any CD30 was expressed on the malignant cells). The third validation cohort was from the County Hospital AIDS Malignancy Project (CHAMP), a prospective database of patients with hematological malignancies and HIV. Of the 100 cases with ARL, only 25 cases were found to have CD30 staining performed, thus only those cases were included. In total, 135 patients diagnosed with ARL were assessed. Cell of origin and germinal (GCB) vs. non-germinal center (NGC) was determined by the Hans algorithm. Statistical differences between groups were analyzed by the fisher exact test. Survival data, when available, was estimated using the Kaplan-Meier method and compared using the log-rank test.
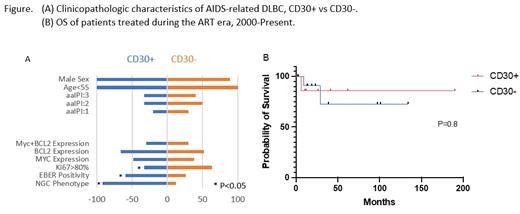
Results: Of the 135 ARL, 30% (n=41) were CD30+. Ninety-one% of the cohort was male. EBER was 23% positive in the entire cohort (n=29/126). EBER was positive in the CD30+ vs. CD30- population, 59% (N=17) vs 26% (p<0.01). Despite 59% of the CD30+ population being EBER positive, 92% of the population had a NGC phenotype, 2% was germinal, and 5% had a null phenotype (p<0.01). Of the 86 patients that were CD30-, 88% were GC vs. 12% NGC (P<0.01). The CD4+ T-cell count at presentation was higher in the CD30- cohort with a mean CD4+ T-cell count of 234 vs.164 cells/ul (p<0.05), similar to historical studies demonstrating a similar effect in germinal vs. non-germinal center ARL. Ki67 > 80% was also higher in the CD30- vs the CD30+ cohort 75 vs.60%, (p=0.052). Myc, BCL2, and double expressor lymphomas were identified 59 vs. 57%, 59 vs. 57%, and 31 vs. 28%, respectively, in the CD30+ ARL vs. the CD30- population, none were statistically significant. Survival data was only obtained for 56 of the patients. In the patients treated in the combined anti-retroviral era (ART), there was no difference in survival in the CD30+ vs. CD30- population, 74% (n=18) vs. 84% (n=12) at 5 years (p=0.8). In the 15 patients treated in the early ART era, the OS at 5 years was 48% for the CD30+ vs. 52% (p=0.4), the rest were treated in the pre-ART era.
Conclusion: CD30+ ARL in this cohort represents 30% of all ARL evaluated, and presents almost exclusively as a non-germinal center phenotype and has a strong correlation with EBV. While no differences in survival were identified in this study, possible due to the small numbers of patients assessed with survival data, historically, NGC ARL have been shown to have poorer outcomes, by 20-30% in studies with da-EPOCH. As such, the need for better therapies, potentially to overcome these poor prognostic factors, should be studied further.
Reid: ADC Therapeutics: Other: Serves as Principle Investigator, Research Funding; Aptose Biosciences: Other: Serves as Principle Investigator, Research Funding; Millennium Pharmaceuticals: Other: Serves as Principle Investigator, Research Funding; Xencor: Other: Serves as Principle Investigator.